The BMJ has just published a study from EPIC – the Norfolk Eye Study, which is well worth reading for all optometrists and those involved in glaucoma care.
The full article is: Glaucoma and interocular pressure EPIC – Norfolk Eye Study: cross sectional study, by Chan et al.
This can be read in full by following the link: EPIC Norfolk Eye Study, BMJ
This was a large scale study with 8623 participants who were assessed for the presence of glaucoma in any form. The age range was from 48 to 92. Patients were screened by IOP measurement, optic disc imaging and visual field testing. Those who showed signs of glaucoma were then examined fully by an ophthalmologist with expertise in glaucoma.

To summarise the results 363 (4%) had glaucoma in one or other of their eyes, of which 314 (87%) were deemed as being Primary Open Angle Glaucoma with either high or low IOP. Of the remainder of the cohort 607 (7%) were found to be ‘glaucoma suspects’ and 863 (10%) were found to be ocular hypertensive.
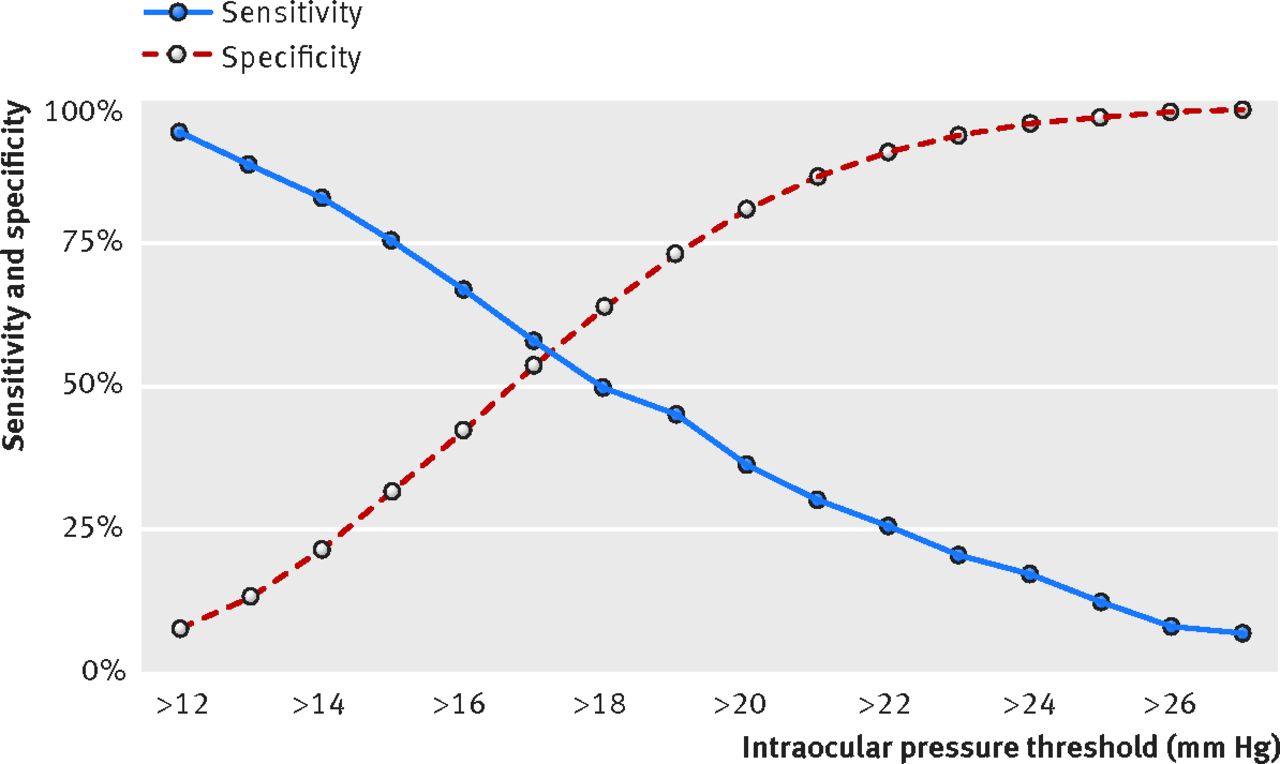
Of those found to have glaucoma, 243 had already been diagnosed – of the 107 patients who were newly diagnosed, 76% had an IOP of less than 21mmHg. When all levels of IOP threshold were checked for their potential as a screening measure – none were found to be useful in terms of sensitivity and specificity.
These are important findings for a number of reasons:
- It helps confirm the fact that IOP as an isolated measure is not a good predictor of whether someone has glaucoma. It is an important measurement as it is our one modifiable parameter through treatment, but it does note have strong value in predicting the presence of glaucoma.
- This helps to highlight the importance of having a good working knowledge of the definitions of glaucoma, and how vital accurate optic nerve head examination and visual testing are in helping to detect glaucoma.
- It highlights that glaucoma represents the sixth biggest condition of all outpatient clinic attendance in the UK, so it places a huge burden in terms of numbers on care providers.
- The burden and challenge of accurately detecting and treating glaucoma is emphasised by the fact that 363 patients in the cohort had diagnosable glaucoma, while over 1400 were either glaucoma suspects or ocular hypertensives. This highlights the huge challenge glaucoma care providers in trying to work through the patient base and evaluating those who have glaucoma or are at significant risk.
- Optometrists both in community and in hospital settings have a very important role in helping to manage this challenge with accurate clinical skills and clear thinking in terms of referral and management decisions.
As mentioned at the top of this short article, this is a very worthwhile read for all practitioners.
Many thanks for reading, and as always all feedback or comments welcome!
Stan


Another excellent article from this guy!
Many thanks Michael!