Welcome to this latest feature article from Optometry-Evolution, in association with Bondeye Optical UK.
Macular degeneration represents a vast proportion of the ocular pathology detected in optometry practice. We have a constantly growing elderly population, so this is always a very relevant area of clinical practice for us to review our skills and knowledge, and ensure that we are doing the very best for our patients.
This article will aim to summarise the two main forms of AMD, how we detect these conditions and how best to manage these patients. It will also touch on some of the current research ongoing to try to develop new treatments.
In recent article from RNIB – they describe that around 2million people in the UK currently experience some degree of significant sight-loss. Of this 2 million, 23% is due to AMD. Currently there are around 370 000 people registered as blind or partially sighted, with AMD being the leading cause. This is a condition that is seen week in, week out by optometrists across the UK. Indeed globally the average life-expectancy is always increasing so the burden of AMD is always increasing.
Dry AMD
This is the most common form of AMD, accounting for over 90% of cases. Prior to anti-VegF treatments becoming available about 10 years ago, this was very much seen as the lesser of two evils, as it was the less aggressive form of macular degeneration. The number of patients who have moderate or advanced dry AMD with significantly reduced visual function, with no current prospect of effective treatment, make this a very significant condition for individual patients as well as a large public health issue.
This form of the disease is characterised by the gradual deposition of metabolic waste products of retinal function under the RPE and within Bruch’s membrane. These are deposits are what we all recognise as being drusen. These occur either in quite discrete forms known as hard drusen, or in larger pale lesions known as soft drusen. These soft drusen are associated with a more progressive form of AMD.
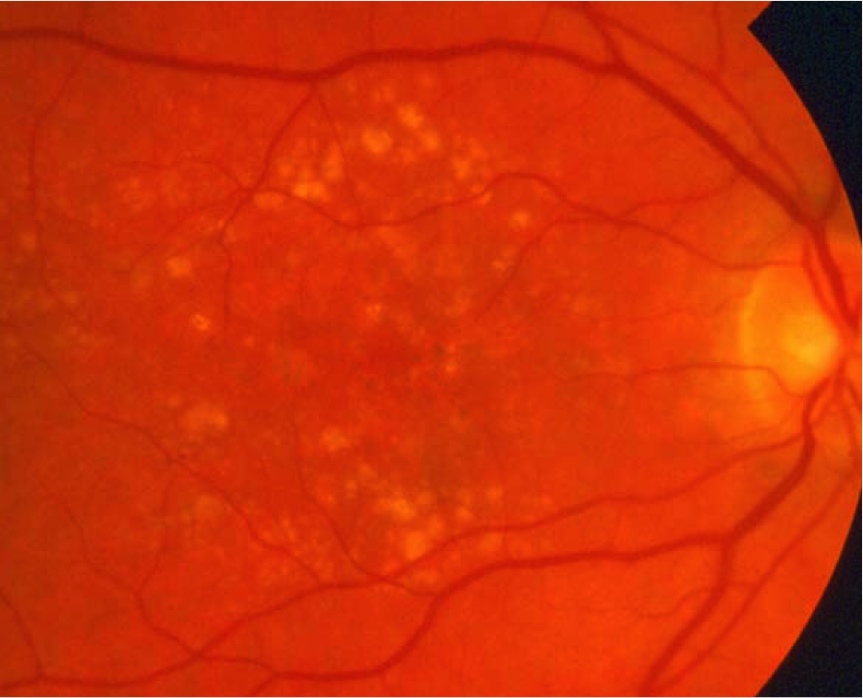
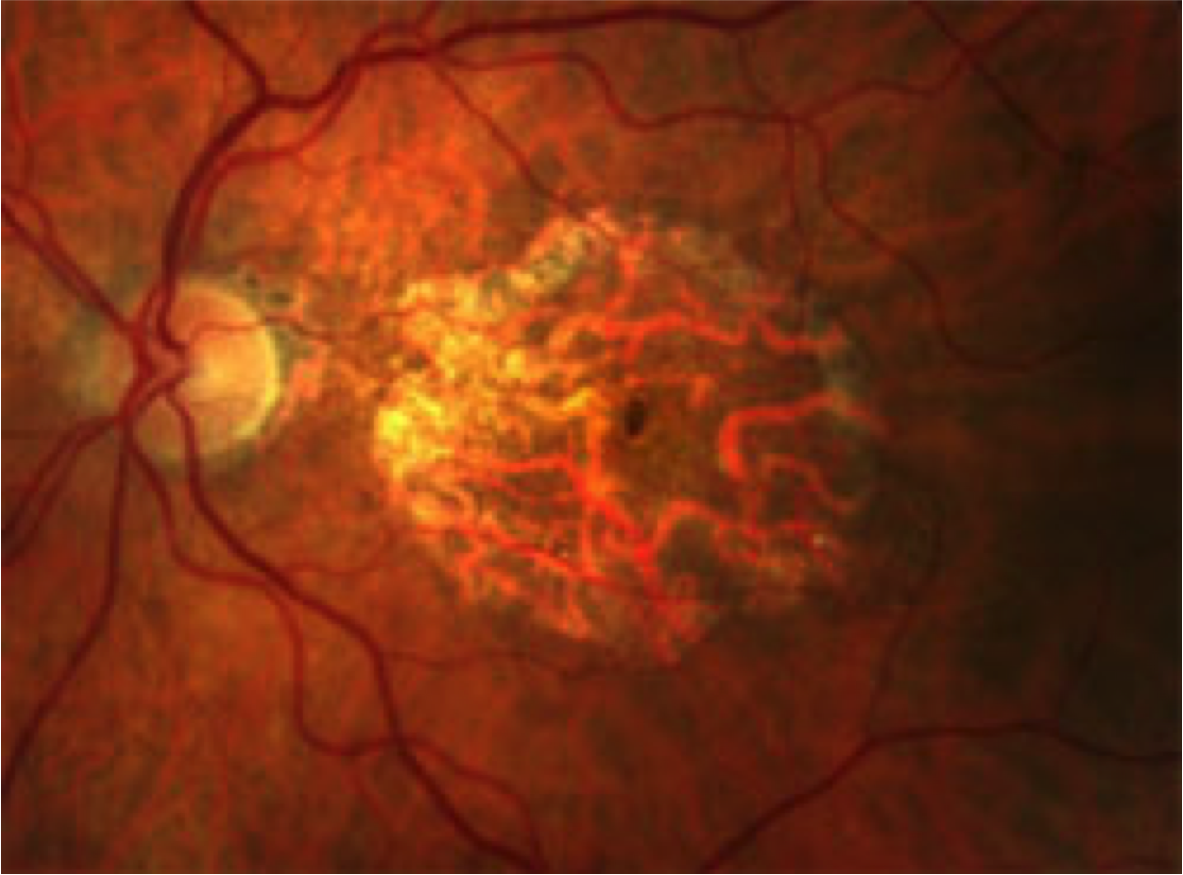
The exact role of drusen in the development of AMD is not fully understood, however they seem to play a part in small atrophic patches forming within the RPE and the photoreceptor layers. These small patches increase in size over time and coalesce to form more significant areas of atrophy, where the normal retinal function is now lost. These can develop into large areas of geographic atrophy encompassing a large proportion of the macular area, by which stage central visual function is significantly damaged. Clinically this will appear as a well demarcated area, often with large choroidal vessels left visible.
This is normally a gradual process that develops over the course of months and years.
Wet AMD
Wet AMD is the more aggressive form of AMD, which tends to develop over days and weeks, so early detection is really important.
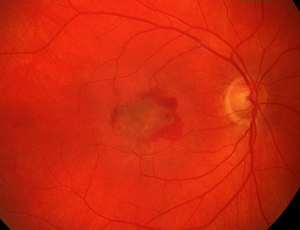
Pathologically there is the formation of a choroidal neovascular membrane (CNV) which can cause leakage of fluid, exudate and haemorrhage into the structures of the retina. This is often facilitated by pre-existing breaks in Bruch’s membrane caused by dry AMD changes.

This formation of a CNV is activated by vascular endothelial growth factor (VEGF). These breaches in Bruch’s may be due to other causes also, such as laser scars, angioid streaks, high myopia or inflammation.
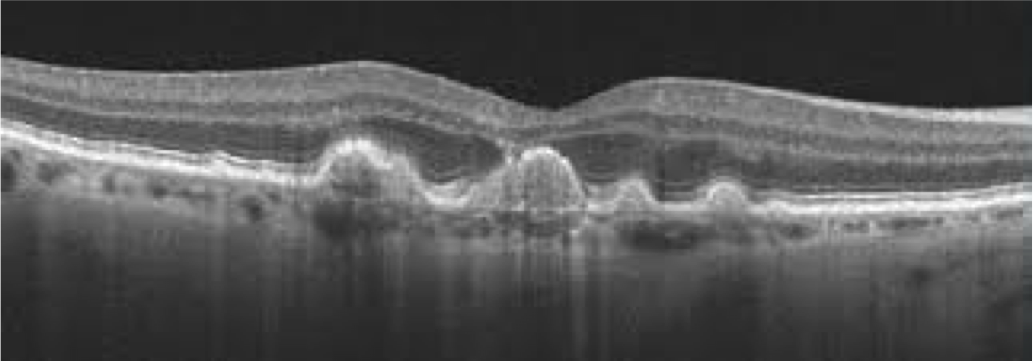
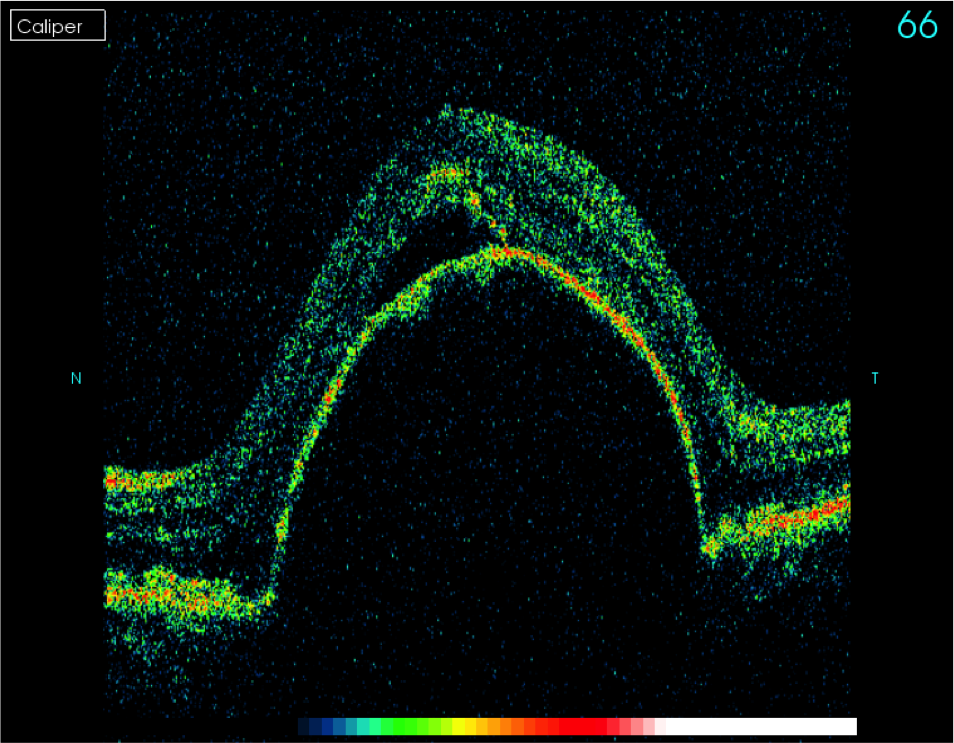
A Pigment Epithelial Detachment (PED) can be a precursor sign to wet AMD. This is a dome-shaped elevation of the retina caused by fluid either building up as a reduced ability of the retina to pump fluid back out tot the choroid, or directly from a CNV. This in itself is not damaging to the vision, however is a significant sign giving its association with wet AMD.
Clinically signs can be subtle, until it becomes more moderate with leakage of blood into the retinal layers. At this point visual damage is likely as the photoreceptors are disrupted, and that blood is toxic to the retina. If this process is allowed to develop, its end point with a large macular fibrovascular scar may be reached.

Patient Examination
Gaining as clear a history of the patient’s symptoms as possible is vital. Dry AMD causes a gradual reduction in central/near vision with reading becoming more difficult over months and years. Print can appear patchy and broken up due to small atrophic patches.
These patients tend not to get metamorphopsia (distortion.) Wet AMD patients experience a more severe and sudden reduction in central vision, ranging in timescale from a few days to several weeks. They very often describe metamorphopsia, where straight lines such as lamp posts or door frames become wavy. Face recognition becoming difficult is a common theme with both conditions.
Visual assessment includes best-corrected distance and near acuity of both eye, and compared to previous measures if available. An Amsler grid can be useful – with dry changes showing up as lines missing whereas wet changes might show up as distorted lines.
Dilated fundal examination with a volk lens is vital to examine the eye in general with a focus on the macula. Only in situations of this being unsafe such as narrow drainage angle should this not be performed.
One key part of this is establishing whether the macula is at all raised. Passing a narrow, focussed vertical beam of light over the macula can help with this. There are several types of lesion that you are looking for which will help establish what form of macular change the patient has. Dry AMD patients might display drusen, areas of hyperpigmentation, patches of atrophy of various sizes. Wet AMD may also have some of these features, however in addition may have a PED, visible haemorrhage or exudate.
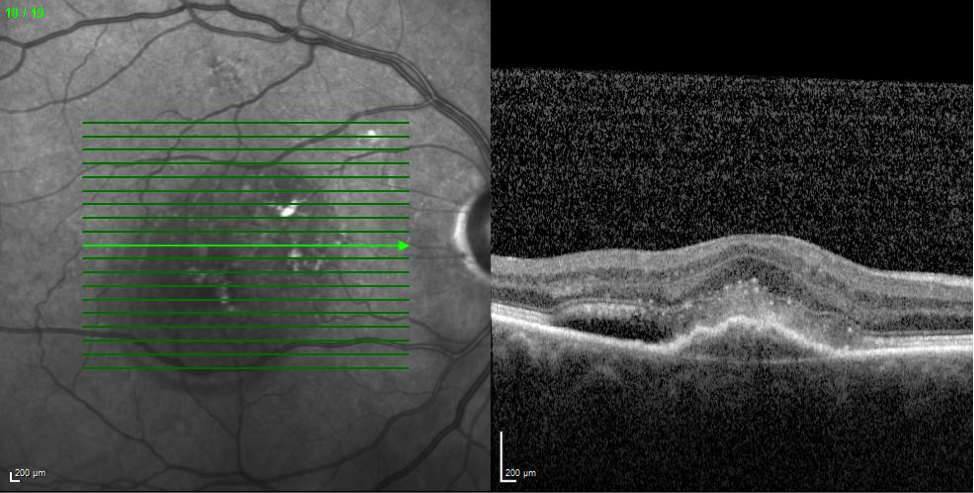
OCT scanning of the macula is really useful in these cases, especially the more subtle wet AMD patients where there may not be any visible haemorrhage. Dry AMD changes can show up in the form of drusen under the RPE, as well as breaches in the RPE. These scans should appear dry with no evidence of fluid. Wet AMD will show fluid at various levels within the retina, including in the subretinal space, and within the retina itself. A PED can show up well also on scanning. CNVs may also be identifiable on OCT.
Anyone using this technology should gain specific education and training on the interpretation of scan results to increase accurate interpretation of these images.
Patient Management
Perhaps the most important element to this is to establish whether the changes seen are purely dry AMD in nature, or whether there is any element of wet AMD which might need referred for consideration of treatment.
Each health board area might have a slightly different mechanism for referral in suspected cases of wet AMD, but usually urgent referral is warranted where there is evidence of wet AMD, particularly with recent onset of symptoms. Patients with end stage disease i.e. with vision below 3/60 and evidence of macular scarring tend not to be amenable to treatment, so it is worth being familiar with your local guidelines on this.
Dry AMD tends not to require referral from the point of view of clinical treatment, however it may still be warranted in cases where diagnosis is ambiguous, where there is ocular co-morbidity such as significant cataract, or are at a level of vision where registration as partially sighted or blind by an ophthalmologist would be appropriate and helpful to the patient. In your area, there may be low visual aid clinics within the hospital so this may another situation where referral would be beneficial.
A couple of useful pieces of advice that you can offer is to help the patient limit the risk factors of AMD. Smoking is one has been shown to increase the risk of developing AMD, and even for patients who have smoked for many years, there is still possible benefits in quitting. Diet and dietary supplementation is another area of interest in AMD. Supplements rich in Lutein and Zeaxanthin, two carotenoids are thought to be useful in reducing the risk of AMD. Eating foods rich in these carotenoids and rich in Omega 3 oils are also thought to be beneficial.
For patients with wet AMD and who ultimately meet treatment criteria, there are now useful treatments in the form of intra-vitreal anti-VEGF injections that can help temporarily shut down the formation of the CNV. In the majority of cases patients require ongoing hospital assessments and injections if or when this process starts up again. This has been a big step forward in the past decade as many patients do respond to these injections and maintain a very useful level of vision, in an eye that previously would have faced inevitable rapid decline in central acuity.
In terms of future treatment potential of dry AMD there is a huge amount of research into modalities such as ‘Complement based therapies’ or ‘Gene therapies’ that try to prevent these changes from occurring, or stem cell treatment which aims to repair damaged retinal tissue. Other visual rehabilitative measures have also been tried such as lens implantation which aims to direct the image onto the next area of healthy retina in relation to the damaged fovea.
From a practical point of view there are a lot of things community optometrists can do to support patients with visual loss due to AMD and this was covered in another article earlier this year on the optometry-evolution website. This can be accessed by following this link: Supporting Visually Impaired Patients in Optometry Practice
There is also a recent follow on the use of modern handheld and stand magnifiers which can be seen on this link: Handheld and Stand Magnifiers – Modern Devices and Their Role
Thanks again for reading – all feedback and comments welcome.
Thank you to Bondeye Optical UK for their support of this article.
If your company would like to get involved in supporting an educational article on optometry-evolution.com, please get in touch.




Excellent summary of AMD and the key features of examination of these patients.