In optometry practice we are quite regularly involved in dealing with eye conditions that have wider underlying systemic associations. We are very good at recognising these conditions and signposting patients either to ophthalmology or their GP, depending on the situation, for blood tests and cardio-vascular risk factors to be investigated, so I thought it might be useful to try to offer a summary of the main tests that are applied to ocular conditions.
I often start any piece of teaching by declaring that I am not an expert, and this short article is a result of doing some extra reading on this topic for my own benefit. Having been more involved in delivery of eye casualty clinics in the hospital over the past few months, arranging blood tests for patients has become a more common occurrence, so it has been a good time to go back and have a read.
This article will offer a summary of the main blood tests that are carried out, and try to highlight the situations when they are relevant in the context of ocular disease.
Blood Pressure
Possibly the most common test of our cardio-vascular function blood pressure can be really useful in a variety of ocular conditions and findings. Some optometrists now have this equipment in practice which makes a lot of sense, as it is a quick and easy test that can be carried out and may help with our onward referral plans for a patient.
There are several situations when measuring the patients blood pressure would be useful – severe headache, swollen optic nerve heads, vein or artery occlusions, hypertensive retinopathy, diabetic retinopathy, or the patient feeling faint or unwell, to name a few.
To summarise, blood pressure measure the systolic pressure over diastolic pressure, where systolic is the pressure at which you heart pumps blood out and diastolic is the resting pressure between beats.

Normal range – between 90/60mmHg to 120/80mmHg
High – over 140/90mmHg
Low – below 90/60mmHg
Blood lipids
This is one of the most commonly performed blood tests looking mainly at the cholesterol levels in the patient’s blood. Again there is quite a wide range of situations when this would be relevant – any retinal circulatory pathology such as blood vessel occlusion or retinopathy, cases of amaurosis fugax or other symptoms suggestive of stroke, any sudden loss of vision or even patients with marked corneal arcus sinnilus with no known cholesterol problems.
Cholesterol is an important component of cellular structures, bile acids and in certain hormones, however high levels of certain forms can be harmful. There are a variety of measurements included in a lipid profile and these are the main ones.
Total cholesterol – common test, and should ideally be below 5, however this measure by itself doesn’t deliver the full picture.
Low Density Lipoprotein – LDL. Otherwise know as ‘bad cholesterol,’ this binds to arteries leading to an increased risk of hypertension and atherosclerosis. Most cholesterol lowering medications target this particular component.
High Density Lipoprotein – HDL. These are our ‘good cholesterols’ and are involved in transporting other forms from the arteries back to the liver.
Triglycerides – again these are harmful and can increase with lack of exercise, high carbohydrate diet and smoking.
Total Cholesterol to HDL Ratio – thought to be a more useful measure as it takes account of our good cholesterols.
Blood Glucose Testing
Diabetes is a range of conditions which results in too much glucose being retained in the blood either through a lack of insulin or resistance to insulin.
Excess glucose can lead to a range of serious acute and chronic complications, with retinopathy being the most familiar to us as optometrists.
The blood testing for diagnosis and monitoring of diabetes consist of the following two main tests:
Fasting Blood Glucose
The amount of glucose retained in the blood several hours after eating
Normal Range – 3.9 to 5.4mmol/l
Pre-diabetic – 5.5 to 6.9mmol/l
Diabetic – above 7.00mmol/l

Glycosylated haemoglobin test (HbA1c)
This is commonly used now as it measures the amount of glucose bound to red blood cells which is thought to give a better average measure of glucose.
Non-diabetic < 42mmol/mol
Pre-diabetic 42-47mmol/mol
Diabetic >48mmol/mol
Blood clotting
This particular test becomes relevant in eye particularly when surgery is planned. A ‘Prothrombin’ (PT) test can be performed, and this is the time it takes for a sample to clot.
This is converted to the ‘International Normalised Ratio’ (INR) which is often tested prior to surgery for patients on blood-thinning medication to assess the risk of excessive bleeding. An INR score of >4.5 suggests a higher risk of haemorrhage.
Full Blood Count
Full blood count gives a snap shot of some of the main blood constituents including Red Blood Cells (RBCs), White Blood Cells (WBCs) and Platelets. This particular test gives an overview of these main groups of cells and platelets with their various subtypes, along with the normal range of values for each.
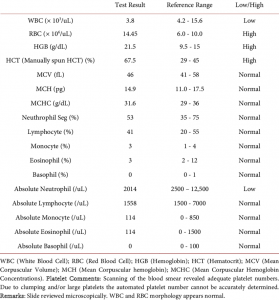
FBC is indicated in a variety of situations such as inflammation which is recurrent, infection or in conditions such as suspected anaemia or leukaemia, which will assess RBC’s and WBCs respectively.
To give a sense of what some of these markers tell us – Neutrophils will be raised if there is an infection of bacterial cause, lymphocytes will be raised in viral infection and eosinophils in cases of inflammation and atopy. Platelets will be raised in cases of infection, significant bleeding and possibly post surgery.
Inflammatory markers
These are a set of tests which help us when we suspect an inflammatory condition such as Giant Cell Arteritis which is a form of vasculitis affecting large and medium sized arteries. From an eye perspective this can crucially affect the blood supply to the eyes leading to Anterior Ischaemic Optic Neuropathy.
The following tests can be used, often in some combination as a part of the investigation of GCA, and other inflammatory conditions.
Erythrocyte sedimentation rate (ESR)
RBCs become positively charged and start to clump together. ESR measure the rate at which these start to settle out after an hour. The normal rates however vary according to age and gender, so this can skew the results to a degree.
C-reactive protein (CRP)
Acute phase protein produced by the liver in response to inflammation or infection.
CRP less affected by other factors such as temperature, medication, age, gender, pregnancy and smoking etc, compared to ESR.
These tests are considered in inflammatory or autoimmune diseases such as Lupus Erythematosus, Sarcoid and Rheumatoid Arthritis.
CRP and ESR can be useful in combination in GCA.
Plasma Viscosity
Testing PV gives an indication of the thickness of the blood which becomes affected by the presence of proteins – which are either present as a part of a normal inflammatory response or proteins produced in an abnormal way due to disease.
Regularly used to aid diagnosis of Polymyalgia and Giant Cell Arteritis and also to monitor these conditions once treatment has been commenced.
Auto-immune Conditions
Diseases whereby antibodies have been developed which can damage the patient’s own tissues.
In eyes we think mainly of conditions such as scleritis, episcleritis, uveitis and retinal vasculitis.
These are some of the main tests relevant to this group of conditions.
Anti-nuclear antibodies (ANA)
Damage tissues by targeting cellular DNA. Common in Systemic Lupus Erythematosus, Sjogrens and Scleroderma.
Rheumatoid Factor (RF)
IgM antibody – increased levels may indicate RA or other conditions such as Sjogrens, Sarcoid and TB.
Human Leukocyte Antigens (HLAs)
HLAs are located are located on the surface of leukocytes, platelets and other cells.
HLA B27 is pertinent to ocular disease – positive in patients with ankylosing spondylitis, Reiters, Crohns for example. Patients who have recurrent uveitis are often tested for this, particularly when there are other systemic symptoms involved.
Angiotensin-Converting Enzyme (ACE)
Patients with Myasthenia Gravis and Sarcoid.
Thyroid function test
Consider for any patient with signs or symptoms of Grave’s disease – proptosis, EOM restrictions, lid retraction, compressive optic neuropathy.
Infectious Diseases
Enzyme Linked Immunosorbent Assays (ELISAs)
- Test to detect certain antibodies in a sample for certain infectious diseases e.g. HIV, Lymes, Toxocariasis
Consider testing for infectious diseases in the following situations:
- Granulomatous anterior uveitis or vitritis
- Retinal cotton wool spots in the absence of Diabetes, High Blood Pressure etc
- Unexplained retinitis or neuritis
Other tests include Renal and Liver function tests that look largely at the various electrolytes and proteins in the blood that may suggest dysfunction of these organs.
This short article only skims the surface of what is a vast topic in itself, but hopefully it has provided a useful overview to the most pertinent blood tests used when it comes to eye disease and gives a sense of their role. There are a whole range of more detailed papers out there looking at these various tests in more detail, and are well worth a read.
Thanks again for reading. Keep a watch out for a CET article in in the coming months looking specifically at GCA as a follow-on to this topic.
Stanley Keys

