Introduction
Welcome to this CET article covering the topic of topical glaucoma medications and their potential adverse effects.
Optometrists are becoming more involved in glaucoma management whether within the hospital setting, specialist clinics or in community based shared care schemes, particularly with the advent of independent prescribing. This article will be a useful for those directly involved in glaucoma care, but also in general for all optometrists to have an awareness of these medications and to be able to recognise when their patients are running into problems with them. This piece will give a brief review of what defines glaucoma, some of the principles as to when to prescribe in glaucoma patients and then the main section looking at each of the four main classes of glaucoma drops. This main section will look at the mechanism of action for these medications and their possible side-effects.
Glaucoma is defined as a group of conditions that cause characteristic progressive damage to the optic nerve head structure, with corresponding functional changes to the visual field. These can occur with or without an IOP raised above the normal standard, with open or closed anterior drainage angles and either as a primary presentation or one with a secondary cause.
An exact diagnosis is therefore made with a combination of tests – anterior chamber examination for secondary factors, gonioscopy, IOP measurement, optic nerve head examination and visual field assessment. Although IOP in itself is not a reliable predictor of the presence of glaucoma, it does provide us with the main modifiable factor which can be targeted as a useful treatment. This applies both to cases with a high initial IOP, or those with a Normal Tension Glaucoma presentation. In some cases treatment may be targeted mainly at opening the anterior drainage angle through laser or cataract surgery.
A host of studies have been published in the past 20 years or so building the weight of evidence that lowering IOP is protective in glaucoma such as the EMGTS and CNTGS studies, and OHTS which looked more specifically at the risk of converting from ocular hypertension to glaucoma. As clinicians we try to make our best judgement as to when to treat patients and how aggressively to do so.
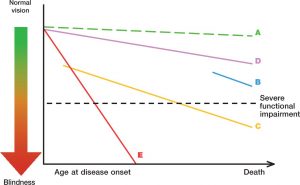
George Spaeth a renowned American glaucoma specialist illustrates this by trying to show the rate or decline of optic nerve function against the patients life –expectancy which can be useful. You can see the various gradients of change, and over time we get a sense for how a patient’s control is behaving with respect to their age, and therefore the likelihood of them running into visual problems due to their glaucoma.
There is also a variety of clinical and patient based factors which help us to reach a decision on whether or not to treat, and these are listed below:
- Patient age, general health and approximate life-expectancy.
- Driving and employment status
- Clinical findings with particular attention to the extent and location of visual field loss.
- Lifestyle – activities
- Ability to cope with instilling drops
- Attitude to taking medication and their understanding of their condition
As a clinician you can see that it is a case of trying to weigh up the clinical evidence of the patient having glaucoma, along with the various patient based factors and the life-time probability that they will suffer visual loss when we are deciding on whether to treat or not, or indeed how aggressively we need to treat.
This article will now move on to look at the different groups of medication available nowadays to lower intra-ocular pressure. The following sections will deal which each group in turn, aiming to describe how they work, and the side effects which can arise in each case.
