The last 10-15years have seen really big steps forward for the optometry profession in terms of our role in detecting and treating ocular pathology. I think it is safe to say that the days of arbitrarily detecting an abnormality and being obliged to refer it for diagnosis are well behind us. The level of diagnostic techniques, technology and clinical qualifications has increased significantly in this time, with optometry being well placed to be the first point of contact for patients with an acute eye condition.
In Scotland the recent amendments to the GOS contract in October 2018 have stated very clearly that optometrists are now obliged to accommodate and examine patients presenting with emergency signs and symptoms. These new regulations state that the optometrist should examine a patient presenting with emergency eye-related problems on the same day or within a reasonable timeframe. In situations where this is not possible they should make reasonable steps for the patient to be examined by another optometrist, GP or hospital department. This is a very clear signal as to where the first port of call is for these patients, so being prepared and equipped for this within practice is vital.
In the rest of the UK MECS and PEARS schemes have been up and running, again with a similar emphasis on accredited optometrists being the first line of patient care. A really encouraging paper in the BMJ last year by Konstantokopoulou et al set out to review the MECS activity and outcomes in two London boroughs. 2123 patient records who were seen in MECS, with 75% being retained in Optometry practice with 19% being referred to HES. 94% of the total were judged to have been managed appropriate while almost 90% of those referred to HES were deemed appropriate referrals. Again this represents a big shift in our profession and the responsibility it is taking on.
Being a hospital based optometrist involved in delivering eye casualty clinics I am more than aware of the pressures on our secondary care systems, so when patients can be managed well in the community it is a huge benefit to the HES across the UK. As our collective skills and knowledge in this area increases with time, so does the quality of referral when patients do actually require to be seen in secondary care. This system however is crucially beneficial to the patients as they can be cared for in the community setting which is often more convenient and desirable than a visit to hospital. From the patient perspective I also sense that their perception of our profession being the first port of call is gradually gathering pace.
When I developed the Eye Emergency Resource Pack, it was very much with this whole shifting tide of emergency eye care towards optometry practice in mind. It struck me that practices will need the tools to be able to respond safely and effectively to these situations of patients presenting with urgent and emergency conditions. This whole patient journey starts with the patient contacting the practice and speaking to one of the practice support team. It is therefore vital for them to be geared up to recognise when patients are reporting signs and symptoms which require prompt investigation, and to play their part in gaining accurate information to help with triaging. I have been greatly encouraged by the feedback from practices who have started using these packs to support their staff in this whole aspect of their role. To date it has been the subject of workshops at several optometry conference, gained a very positive review in Optician Magazine and has been gaining interest with LOCs and AOCs wishing to tap into these resources for their member practices.
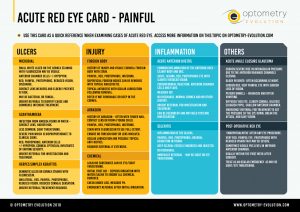
More recently I developed a card called the ‘Acute Red Eye Card’ for optometrists, as this will be one of the main areas of acute and urgent eye care they will be faced with. This summarises the main acute presentations, highlighting the main situations where there is something more serious at play.
The continuous changes in our profession I find really exciting. Being able to detect and in a lot of cases treat patients at source in optometry practice is a genuinely positive development for patients, but also for optometrists. This opens up their scope of practice, particularly when they are IP qualified, making their role more clinically diverse and rewarding. Who knows what the next 10-15 years will hold?
Thanks for reading.
Stan